Blog Information
- Posted By : Thomas Schmitt
- Posted On : Apr 30, 2024
- Views : 405
- Category : NFL
- Description :
Overview
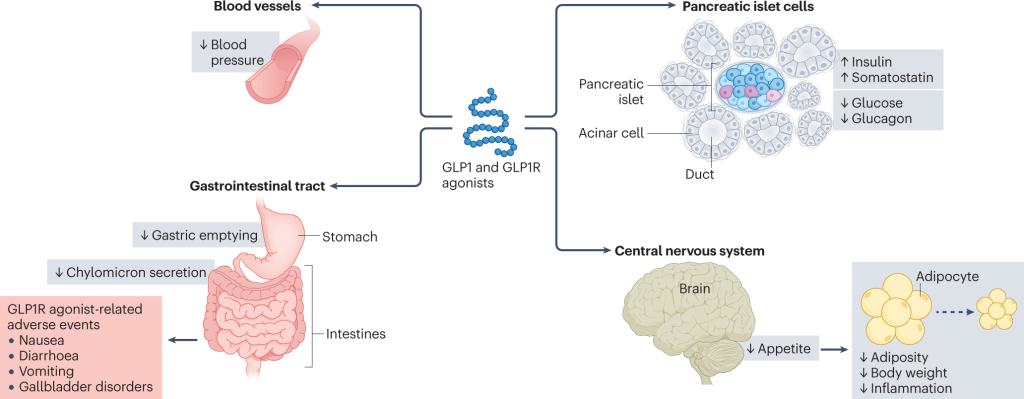
The incidence and prevalence of diabetes are increasing year by year globally, and patients with diabetes are at increased risk of cardiovascular disease and heart failure. Diabetic cardiomyopathy (DCM) refers to the presence of abnormal myocardial structure and performance in the absence of other heart-related risk factors (such as coronary artery-related disease, hypertension, and severe valvular disease). DCM can lead to cardiac systolic or diastolic dysfunction, further causing heart failure with reduced ejection fraction and heart failure with normal ejection fraction, seriously affecting the patient’s quality of life. The pathogenesis of DCM is particularly complex. Current research has discovered multiple mechanisms of action, including metabolic disorders, insulin resistance, formation of advanced glycation end products, mitochondrial damage, oxidative stress, endoplasmic reticulum stress (ERS), Inflammatory response and cell apoptosis, etc. Glucagon-like peptide-1 (GLP-1) receptor agonist is an incretin secreted by intestinal L cells. It reduces the blood sugarof diabetes in patients with diabetes by increasing glucose-dependent insulin secretion and inhibiting glucagon secretion, and also regulates a variety of cardiovascular risk factors, thereby inhibiting the process of atherosclerosis and reducing the occurrence of coronary events and cardiovascular death. GLP-1 receptor agonists have a longer half-life, are more effective than many oral hypoglycemic drugs in clinical trials, and have a low risk of hypoglycemia. This article reviews the effects of GLP-1 receptor agonists on DCM to provide reference value for further research on GLP-1 receptor agonists.
Figure 1. Major cardiometabolic actions of GLP1.
GLP-1 Receptor Agonists Affect DCM by Regulating Metabolic Disorders
Hyperglycemia and insulin resistance are the most significant features of DCM. In addition, they are also accompanied by changes in myocardial structure and function caused by calcium imbalance, abnormal lipid metabolism, lipid deposition, and the combined effects of multiple hormone changes. The metabolic disorder of myocardial cells is mainly caused by the increase in blood sugar levels caused by insulin resistance. When diabetes occurs, there are conversion obstacles in both the anaerobic glycolysis and aerobic oxidation of glucose in the body. The body’s utilization of glucose is reduced, lipolysis is increased, and excessive free Fatty acids are absorbed by cardiomyocytes, reducing the heart’s ability to use glucose. At this time, the heart mainly relies on fatty acid oxidation to provide energy, but high oxygen consumption is accompanied by low energy metabolism efficiency. The accumulation of free fatty acids in the form of triglycerides promotes fatty degeneration of the myocardium. Therefore, long-term hyperglycemic environment, abnormal lipid metabolism, and lipid deposition lead to the occurrence and development of DCM in diabetic patients. Multiple studies have shown that GLP-1 receptor agonists can directly or indirectly improve the function of cardiomyocytes by controlling the above multiple metabolic factors and related signaling pathways.
GLP-1 Receptor Agonists Affect DCM by Improving ERS
In diabetic patients, the endoplasmic reticulum dysfunction caused by cardiac oxidative stress, abnormal lipid metabolism and inflammatory response is called ERS when the body is in a high glucose state. Pathophysiological factors such as ischemia, hypoxia, oxidative stress, or calcium homeostasis disorders can disrupt endoplasmic reticulum homeostasis, cause endoplasmic reticulum dysfunction, and lead to the accumulation of unfolded or misfolded proteins, thus inducing ERS and triggering unfolded protein response, thereby activating the corresponding endoplasmic reticulum and calcium regulatory mechanisms and other signal transduction pathways to restore endoplasmic reticulum homeostasis. When the ERS intensity is too high or lasts for a long time, the endoplasmic reticulum cannot restore homeostasis. At this time, multiple pathways induce cell apoptosis, which together with multiple factors lead to cardiomyopathy and heart failure. Increasing evidence shows that ERS is associated with diabetes, endothelial dysfunction, and atherosclerosis. GLP-1 receptor agonists can inhibit ERS and reduce intracellular calcium concentration through indirect effects, thereby reducing myocardial damage. Their effects may be related to the inactivation of the ERS signaling pathway.
GLP-1 Receptor Agonists Affect DCM by Interfering with Inflammatory Response
Oxidative stress is an important factor driving the inflammatory response. High glucose status and insulin resistance in diabetic patients promote cell metabolism disorders and release a large amount of reactive oxygen species, which in turn activates nuclear factor κB, induces the expression of inflammatory factors, damages vascular endothelial cells, and causes abnormal proliferation of smooth muscle cells. It will affect the structure and function of the heart in the long term, leading to the occurrence and development of DCM. GLP-1 receptor agonists can inhibit the inflammatory pathway through direct or indirect effects, activate the AMP-activated protein kinase (AMPK) pathway, reduce the activity of nuclear factor κB, reduce the production and release of inflammatory mediators, inhibit the differentiation of inflammatory monocytes and macrophages, and Reduce heart and blood vessel inflammation, etc.
GLP-1 Receptor Agonists affect DCM by protecting Mitochondria and Improving Oxidative Stress
The tissue damage of DCM mainly has the following five mechanisms: (1) Increased metabolism of glucose and other sugars through the polyol pathway; (2) Formation of intracellular advanced glycation end products; (3) Advanced glycation end products Increased expression of receptors and ligands; (4) activation of protein kinase C subtype; (5) overexpression of hexosamine pathway activity. Mitochondria are one of the main sources of reactive oxygen species in cardiomyocytes, and reactive oxygen species are the upstream products of the above five pathways. In the body’s high-glucose state, due to changes in metabolic substrates, the oxidation of free fatty acids increases the transfer of reducing equivalents, which can damage the ability of the electron transport chain, increase the generation of reactive oxygen species, excessive reactive oxygen species deposition, or weaken the antioxidant mechanism. The redox imbalance leads to oxidative stress; this process and the high glucose state can simultaneously promote oxidative stress and the body’s inflammatory response, damage myocardial cells, and then lead to myocardial fibrosis, ventricular hypertrophy, coronary microvascular damage, cardiac systolic and diastolic function obstacles, eventually developing into DCM. In the entire pathogenesis of DCM, the effects of GLP-1 receptor agonists on metabolic disorders, accumulation of reactive oxygen species, ERS, and inflammatory responses all require the oxidative stress link. The oxidative stress link can be called the key to the pathogenesis of DCM. Therefore, intervening in the oxidative stress process is an important step in improving the prognosis of DCM. Studies have shown that exenatide reduces oxidative stress in cardiomyocytes and improves mitochondrial function by activating autophagy; it can also remove dysfunctional mitochondria to inhibit cardiomyocyte apoptosis, achieve anti-apoptosis and antioxidant effects, and protect cardiac function. Exenatide can also inhibit the activation of caspase-1, indirectly attenuating mitochondrial damage and reducing reactive oxygen species deposition, thereby attenuating oxidative stress.